TUBULAR STRESS - a kidney drama
- docbinah
- Jan 14
- 3 min read
By Robin Rose MD January 15, 2026

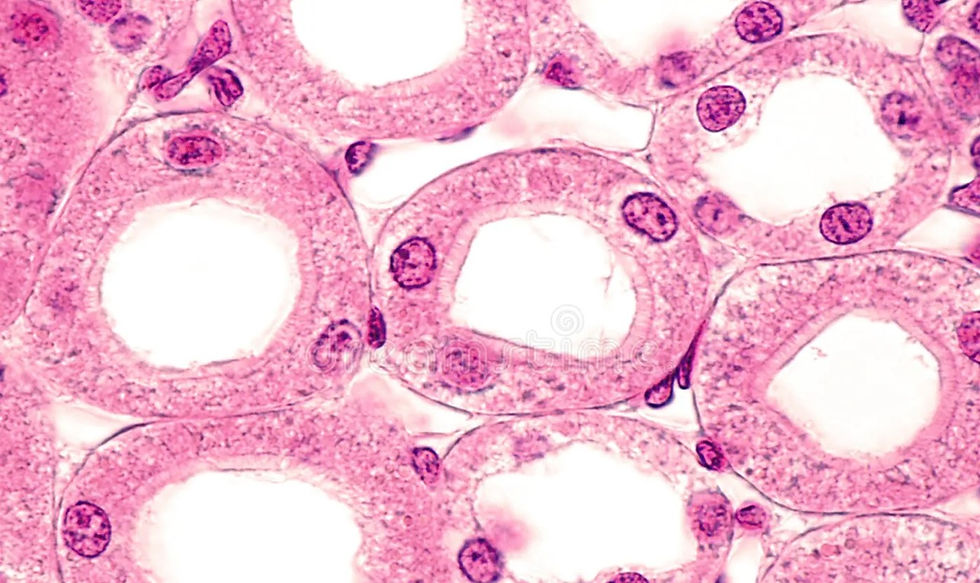
👉🏿🌿🌿 Kidney Tubules are where the action is!!
Even in glomerular diseases, declining tubule status is critically important and often precedes the other damages that harm kidney and disrupt filtration in the glomerulus.
Tubule wisdom has become a passion for me in the RENOLOGY journey - the earlier we can step in with awareness of what’s causing kidney decline the more our regenerative medicine wisdom can shine.
So let’s learn together.
“TS” IS TUBULE STRESS.
🌿👉🏿👉🏿What TS-staging means
(core concept)
TS-stage = Tubular Stress stage.
This is a functional- physiologic- metabolic process and concept that complements (and often precedes) eGFR/albuminuria by focusing on tubulointerstitial biology—where CKD usually begins and accelerates.
✨GFR tells you what’s already lost.
✨TS-stage tells you what’s under attack now—and still salvageable. That is a handle for kidney success.
👉🏿🌿🌿Why TS-staging is needed
Conventional CKD staging:
Overweighs glomerular filtration
Misses early tubular injury
Labels Stage 2 decline as “aging” or “normal”
Detects disease late (missing windows for regenerative possibilities)
TS-staging reframes CKD as:
✨A toxic–metabolic–hypoxic disorder of tubules
✨Driven by SNS tone, phosphate load, acid stress, inflammation, toxins
✨Often present years before creatinine rises
👉🏿🌿🌿TS-Stage framework
—-::>>> (TS0 → TS4)

🌀TS0 — Tubular Reserve (the Resilient Kidney)
👉🏿Biology
Intact proximal tubules
Normal mitochondrial density
Adequate renal perfusion
👉🏿Labs / signs
Normal bicarbonate
Normal phosphate handling
Low/normal FGF-23
No tubular protein markers
👉🏿Clinical
High renal reserve - healthy!
Stress-tolerant (capable of handling the trauma of illness, meds, toxins, and dehydration)
🌀TS1 — Early Tubular Stress (Reversible)
👉🏿Biology
Mitochondrial strain
Oxidative stress
Early transporter dysfunction
👉🏿Clues
Mild non–anion gap metabolic acidosis
Phosphate creeping up within normal range (remember in RENOLOGY - phosphorus >3.5 mg/dL is already creating metabolic havoc )
Rising FGF-23 with normal PTH
Fatigue, cold intolerance, nocturia
👉🏿Key point
Creatinine often still normal
This is the sweet spot for prevention
🌀TS2 — Established Tubular Injury
👉🏿Biology
Brush border injury
Impaired ammoniagenesis
SNS-mediated vasoconstriction
👉🏿Markers
↓ Bicarbonate
↑ FGF-23, ↓ Klotho activity
Tubular proteins (β2-microglobulin, RBP, NGAL)
Early phosphate toxicity
👉🏿Clinical
eGFR may still be “Stage 2”
Exercise intolerance
BP lability
Increased toxin sensitivity
👉🏿👉🏿👉🏿TS2 ≠ normal aging
👉🏿This is active kidney disease.
🌀TS3 — Tubulointerstitial Fibrosis (Progressive)
👉🏿Biology
Capillary rarefaction
Fibroblast activation
Reduced oxygen diffusion
👉🏿Findings
Persistent acidosis
Mineral bone axis distortion
Worsening SNS tone
Sarcopenia / visceral fat loss
👉🏿Clinical
eGFR decline accelerates
Poor recovery from illness
Medication intolerance
🌀TS4 — Tubular Exhaustion (Low Recovery Potential)
👉🏿Biology
Fixed fibrosis
Loss of adaptive capacity
👉🏿Clinical
Narrow therapeutic window
Frequent decompensation
Focus shifts to preservation and symptom stability
A patient can be:
CKD Stage 2 + TS3 (dangerous, ☠️often missed)
CKD Stage 3 + TS1 (salvageable)
👉🏿🌿🌿Key drivers of TS-progression
Phosphate load / FGF-23 rise
Chronic SNS activation (renalase axis)
Low-grade acidosis
Visceral fat loss / catabolism
Environmental toxins (mold, metals, solvents)
Hypoxia / sleep disruption
👉🏿🌿🌿Clinical use:::
(how TS-staging changes medical care)
🌀TS-staging informs:
Nutrition (phosphate density, protein timing)
Hydration type (not just volume)
Peptide / bioregulator selection
Exercise dosing and commitment
Sleep normalization
Medication tolerance
Illness risk stratification
🌀It answers:
“How stressed are the tubules right now?”
—not just “What is the GFR?”

👉🏿🌿🌿Practical TS-staging inputs (clinic-ready)
Serum bicarbonate trend
Phosphate
FGF-23
Urinary tubular proteins
BP variability / orthostasis
Body composition (VAT loss)
Symptom pattern (fatigue, cold,
👉🏿🌿🌿CONCLUSION
TS-staging reframes CKD as a dynamic, tubular-centric process—::> detectable early, modifiable in mid-course, and preventable from accelerating when addressed correctly. Kidney success!
🔆THAT’S RENOLOGY!!🔆




You r a special person Robin ! Many Many thanks! ❤️🥰❤️
Thank you from the bottom of my heart.
This makes me feel able to have a balance plan to encourage healing.